The Power of Positive Self-Talk: Rewiring Your Inner Dialogue
The ongoing conversation you have with yourself every day - self-talk - can motivate and remind you of your strengths and abilities. Other times, it may be like a critic pulling you down with self-doubt. The way you talk to yourself can affect how you view yourself, the world around you and handle problems.
However, paying attention to your thoughts and steering them to positive self-talk can greatly improve your confidence, productivity, and quality of life. Let’s discuss some helpful tips.
How Positive Self-Talk Works
The essence of positive self-talk is not to ignore reality or embrace self-delusion. Rather, it involves consciously using encouraging and supportive words in thoughts or inner conversations about yourself or your situation.
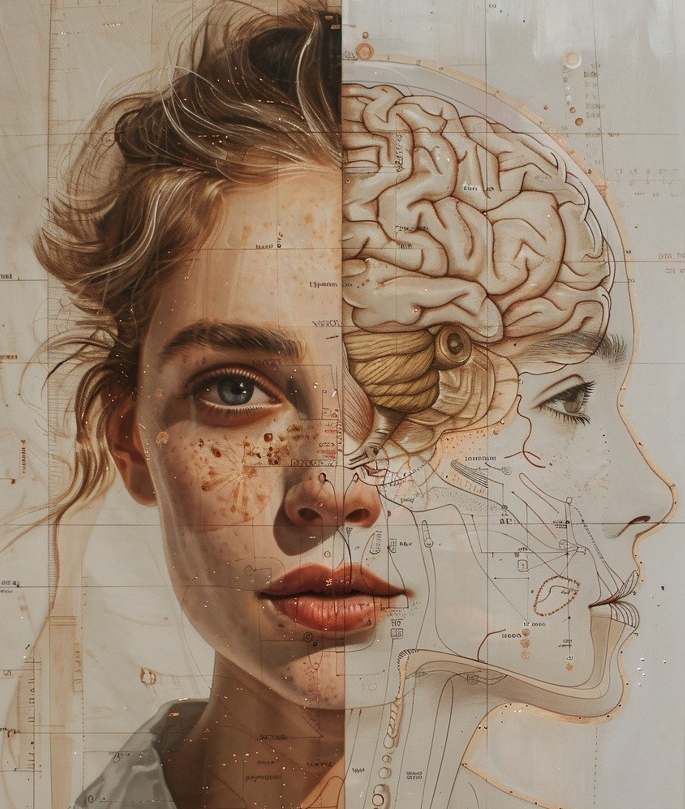
Interestingly, the human brain is remarkably adaptable and it strengthens the connections it uses most frequently. So, If you have a habit of positive self-talk, that’s what your brain will support and your thoughts will naturally lean to more constructive and empowering thoughts.
I have learned from experience that positive self-talk can be like a supportive friend that helps me face challenges with determination. For example, whenever I experience self-doubt, especially during big transitions, telling myself, “I’ve handled tough situations before, and I can do it again” has provided a sense of calm and confidence. By actively practicing positive self-talk, I noticed a shift not just in my thoughts but also in my actions. I now approach challenges with a mindset of growth rather than fear of failure.
Rewiring Your Inner Dialogue
In reality, an optimistic mindset doesn’t happen overnight. Rewiring your inner dialogue is a process, and like most processes, it requires effort. But with time and consistent practice, positive self-talk becomes more natural.
Here are some helpful tips:
Notice your self-talk
Start by paying attention to the things you say to yourself throughout the day. After all, awareness is the key to making any change. So, check whether your thoughts boost your confidence or encourage self-doubt.
Challenge negative thoughts
Honestly, not every thought is real. Sometimes, the mind disguises fears and assumptions as facts. Also, dwelling on upsetting events and past mistakes can fuel negative thoughts. So, check the accuracy of your thoughts whether you are overthinking, overreacting, or even overgeneralizing. Most times scrutinizing our negative thoughts helps weaken their influence.
Replace negativity with positivity.
When your inner voice tells you, “I can’t,” replace it with something like, “I’ll find a way.” Or when your mind tells you “I’m a failure,” tell yourself, “I’m growing, and I’ll get better.” Switching negative phrases with more empowering ones can slowly rewire your brain to think more positively.
Practice Gratitude
According to Plato, a grateful mind is a great mind which eventually attracts to itself great things. Gratitude makes it easier to embrace a positive mindset. Focusing on what’s good, even in the tiniest of things, can help you retrain your brain to see possibilities instead of problems.
Positive Self-Talk Matters
Our thoughts shape our reality. If your inner conversations promote self-doubt and negativity, it can keep you from reaching your full potential and increase stress and anxiety. However, when you consistently practice positive self-talk, you’ll notice changes in your actions and feelings. You will feel more confident, approach challenges with optimism, and when things don’t go perfectly, be more forgiving of yourself. Over time, this change in mindset will help you have better mental health, stronger relationships and a greater sense of fulfilment.
In today's image-driven culture, some individuals turn to plastic surgery in an effort to align their appearance with societal ideals or personal expectations. While there’s nothing inherently wrong with wanting to enhance one’s physical features, it's important to examine the self-talk behind that decision. Are you speaking to yourself from a place of self-acceptance, or from harsh self-criticism? Positive self-talk doesn’t mean rejecting change, but rather ensuring that any change — even cosmetic — stems from self-love and not self-loathing. This mindset helps ensure that external changes complement, rather than compensate for, your internal sense of worth.
Conclusion
Rewiring your inner dialogue isn’t just about thinking happy thoughts. Be intentional. With positive self-talk, you become your own biggest supporter and create a more supportive, and compassionate mindset that helps you thrive. That inner support can make all the difference in how you face life’s challenges.